Recently Tested Positive for SIBO (or Suspect you Have it)? Here’s What Else you Need to Consider Beyond Treatment (so you Don’t End up with it Again)
If you’ve been diagnosed with SIBO, or suspect you have it — you’ll know that it means you have an overgrowth of bacteria where they’re not supposed to be (the small intestine).
And that it can contribute to a whole slew of symptoms:
The GI stuff like bloating, gas, tons of food sensitivities, irregular bowel movements (typically constipation, diarrhea, or a mixture of both depending on which subtype of SIBO you have), reflux
AND things like skin issues (eczema, rosacea, rashes), histamine issues/intolerance (and associated symptoms), weight fluctuations, anxiety, depression, migraines
Sheesh 🙄
Something else that’s important for you to be aware of though, is that SIBO is not a root cause.
Sure, it can drive the above mentioned symptoms
But SOMETHING made the environment in your small intestine conducive to the overgrowth
And it’s that upstream, deeper root-cause that needs to be investigated and addressed, if you want to ensure that your SIBO eradication is both successful, and long-standing
Recurrence rates of SIBO are high (it’s thought that within the first year post conventional treatment, SIBO recurrence rates may be as prevalent as 40-60%), and I don’t want you going through all the hard work involved in getting rid of your SIBO to just end up right back with it again.
So let’s explore some of the common upstream “root causes” of SIBO for you to consider, investigate, and remedy so that you can kiss your SIBO goodbye!!!
Support your Gut Motility
SIBO is primarily a motility disorder. Motility referring through the careful coordination of functions (like muscle contraction) that MOVES stuff through the GI tract (food, metabolic waste, dead cells, microbes, etc).
When our digestive system isn’t moving along in an efficient manner — our small intestine can become more conducive to overgrowth.
Foods hangout longer, which gives the bacterial populations that DO inhabit the small intestine more time to eat and reproduce and proliferate
AKA we get bacterial overgrowth
As such, supporting healthy gut motility is critical here!
Motility issues, or “dysmotility” can occur due to poor thyroid function (more on that below), unconducive lifestyle habits, diabetes, traumatic brain injury, infections (gut infections, mold), dysautonomia, and post-infectious IBS (more on that in a bit, too!).
A term you might hear that’s part of this whole gut motility picture is something called the “migrating motor complex”
This is the wave-like motion of muscle contractions that moves throughout our GI tract periodically throughout our days, moving everything along
Supporting the migrating motor complex through some simple strategies is a great place to start if you have SIBO or suspect you have it based on your symptoms (or honestly, if you struggle with digestive issues like bloating, gas, distention, and constipation in general).
One of my favourite things to recommend to clients to support healthy gut motility and the migrating motor complex is through MEAL SPACING
Spacing your meals and snacks at least 3-4 hours apart is critical for proper MMC (migrating motor complex) function, as the MMC only occurs when the body is in a fasted state. So between meals (AFTER we’re done digesting), and overnight.
If you’re a snacker or a grazer, or you just tend to eat more frequently than every 3-4 hours, I’d urge you to slowly start creating more time between and notice how much it has an impact on your digestive symptoms (not to mention how important this is for SIBO prevention!).
Look into your Thyroid Function
Our thyroid plays key roles in digestion.
Healthy thyroid function plays a critical role in motility and digestion. Thyroid hormones directly impact our gut motility and determine the coordination of smooth muscles in the GI so things can move along efficiently!
When thyroid function is poor, and thyroid hormone conversion is inadequate, our digestion becomes impacted. Poor thyroid function slooooows everything down.
This can lead to digestive symptoms like constipation, distention, bloating, gas. It can also leave us more susceptible to developing SIBO.
Things become more stagnant; and as per above, when stuff’s not moving through our small intestine efficiently, those microbes will be quick to take advantage
Investigating your thyroid is a key component of the SIBO picture. Don’t sleep on testing your thyroid!! Particularly, a comprehensive thyroid blood panel.
Often when we go to our providers for thyroid testing, they’ll just run TSH (which is a pituitary hormone, called thyroid stimulating hormone)
This doesn’t give us the full picture, however, of how overall thyroid function might look. We want to see TSH, we want to see the hormones that the thyroid produces (T4, T3), we want to see reverse t3 (a conversion product), annnnd antibodies which gives us information on thyroid autoimmunity
Here’s the panel to ask your practitioner for: TSH, tT4, fT4, tT3, fT3, rT3, TPO, TgAB
If you have suboptimal thyroid function, hypothyroidism, Hashimoto’s, AND you know or suspect you have SIBO, bringing thyroid support to the forefront is a must!
Support Proper Digestion
If your digestive system isn’t working properly, in that you have low digestive OUTPUT: not enough stomach acid, bile, or pancreatic enzymes are being secreted to digest properly, again we can be left with an environment in the small intestine that’s more conducive to overgrowth.
Stomach acid is the conductor of digestion. And it’s commonly compromised!
Chronic stress, nutrient deficiencies, a history of (or current) PPI use, and H.Pylori infections are all common causes of poor stomach acid output that I see often in my clients.
It’s one of our first lines of defence against pathogens and bad bugs we may be exposed to. It’s a key part of our digestion in the stomach. It’s what signals the production of digestive enzymes and bile (so that we can further breakdown our food once food makes it to the small intestine).
Without adequate stomach acid levels, we don’t have that level of protection, digestion suffers, and we don’t get proper signaling more downstream. It’s a whole cascade that can be really problematic, and can absolutely set the stage for SIBO to develop!
Prioritize digestion through nutrition and lifestyle strategies (getting in the nutrients required to produce stomach acid, prioritizing meal hygiene, chewing really well), and considering herbal and supplemental supports as it makes sense for you and your case (like digestive bitters, betaine HCl, digestive enzymes, bile).
*Note this is not medical advice; please check in with your practitioner prior to trying any supplementation as there may be contraindications or interactions with health conditions/meds/etc.
Support Healthy Bile Flow (Especially if you Don’t have a Gallbladder)
This is along the same wavelength as the last section (ie. supporting digestive function), but I want to zero in more specifically on bile support.
Without your gallbladder, your physiology changes. Yur digestion and detoxification changes.
Bile is a substance that’s made in the liver, and stored and concentrated in the gallbladder. It’s secreted in response to eating, to work on fat digestion.
I go into bile, gallbladder, and liver health much more in depth in this article here; definitely go check it out.
But what’s important for you to know here is this: bile can impact our motility and leave us susceptible to SIBO twofold.
Bile has natural antimicrobial properties that helps to keep populations in the small intestine managed. Without it, or without it in such concentrated amounts, the microbes in the small intestine can start to proliferate
It has natural “laxative-like” properties, helping to promote efficient gut motility and healthy bowel movements (sometimes, post-op clients swing constipated because of the lack of bile flow that occurs)
If you don’t have a gallbladder, and suspect/know you have SIBO, consider bile flow support as part of your overall strategy (of course depending on what your symptom presentation looks like; if you have BAM, or diarrhea as a result of bile dumping, this will not be applicable to you right now).
This will probably include bitters foods, and foods and herbs that support bile production and healthy bile flow/viscosity.
This may also include things like digestive bitters (as a tincture), and potentially supplemental supports like ox bile and/or TUDCA (talk to your practitioner about whether either or both of these are right for you!).
Assess for Structural Issues
Structural issues like adhesions, scar tissue, faulty valves, endometriosis, strictures, fistulas, a history of abdominal surgeries, short bowel syndrome, etc., can all contribute to motility issues and an environment that’s more conducive to SIBO.
Being mindful of your health history, getting proper diagnostic screening done, and even seeing a manual practitioner (who can work on scar tissue, for example), are all great ideas here.
Ileocecal Valve Dysfunction
The ileocecal valve is a sphincter that connects the small intestine to the large intestine. It’s located on the lower right side of your abdomen, sort of halfway between your right hip bone and belly button. This is where your small and large intestines meet.
If you remember, the large intestine is where the majority of our microbiome reside. In the small intestine, we have VERY minimal amounts of microbes compared to our colon.
This valve/sphincter muscle is meant to flow ONE way: from our small intestine INTO the colon.
When this valve becomes dysfunctional, or relaxes/doesn’t close properly, it can allow backflow of contents (ie. microbes!!), from the large intestine into the small intestine, which can drive SIBO.
Seeing a manual practitioner who can do visceral manipulation can be really helpful here.
Address Stress
I know I know.
But I have to mention it here, because it does (unfortunately) play a big role in not just SIBO, but digestive issues in general.
Stress (of the chronic variety), shuts down digestion. It lowers stomach acid output. It impacts the gut-localized immune system. It impacts bile and enzyme output. It redirects blood flow AWAY from our digestive system, and towards our extremities, which doesn’t help us from a digestive function perspective.
I know stress, and stress management, and building resilience is a layered, nuanced topic, but as far as your SIBO is concerned, do your best to do what you can here.
Some of my favourite tools for stress management (outside of actively trying to remove stressors from your life wherever and however possible), are:
breathwork in all its forms (4-7-8, physiological sigh, box breathing, resonance breathing, alternating nostril breathing)
bilateral stimulation
EFT tapping
time in nature (ideally without devices)
boundaries with social media/technology (been loving the Brick for this!!)
heartmath
walking
any creative hobby: scrapbooking, painting, sketching, knitting
acupuncture
massage
non-sleep deep rest
vagal-toning exercises
See if one or two of these resonate with you, or peak your interest, and see about building them into your daily routines!
Ever got Food Posioning/Gastro? Consider Post-Infectious IBS
If you’ve had food poisoning, or gastroenteritis, and noticed your symptoms started or worsened afterward (could’ve been soon after, or some time after), there’s potential that PI-IBS is at play for you, especially if you’ve had recurring or stubborn SIBO.
Post infectious IBS is autoimmune in nature. Hence it being behind a lot of stubborn-can-never-seem-to-clear SIBO cases.
There’s a response that can occur off the back of food poisoning/gastro, where the immune system starts to attack a toxin released from the pathogens causing the gastro.
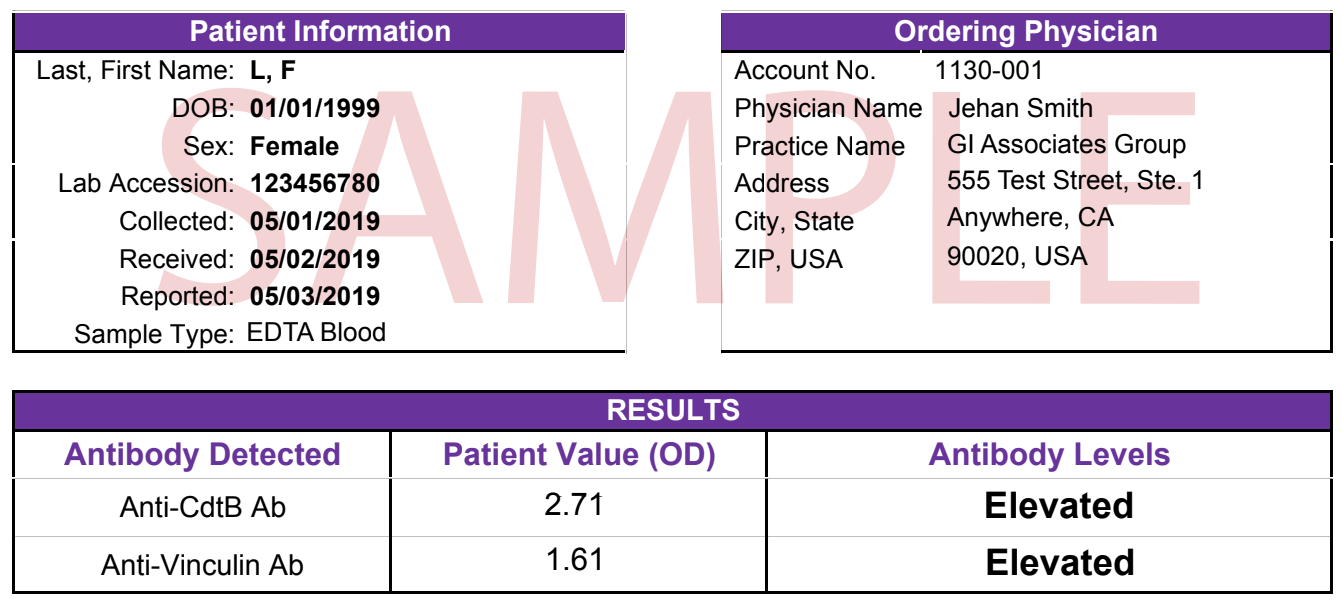
The immune system can ALSO attack a naturally occurring protein found in our bodies, called vinculin, that plays a role in gut motility. The toxin produced by pathogens (CdtB) and vinculin look super similar — hence the inappropriate attack from our immune system.
Eventually our body creates an antibody to vinculin (called anti-vinculin), and its THIS antibody that can cause nerve damage and compromise gut motility, which can lead to SIBO and associated symptoms.
If recurring SIBO is something you’re dealing with, consider running an IBS-Smart test to investigate this!
Image of sample report from: https://www.rupahealth.com/lab-tests/gemelli-biotech-ibs-smart
Consider your Medications
Meds can be part of this picture, too!
Certain medications can play a role in SIBO development due to their impact on gut motility.
Consider:
PPI’s (proton pump inhibitors) that lower stomach acid output (see above for how low stomach acid levels can contribute to SIBO and other digestive concerns)
A history of antibiotics (that can disrupt the gut microbiome and our gut motility)
Even Levothyroxine (which is one of the most commonly prescribed thyroid medications (T4) can keep us susceptible to SIBO if it’s not being converted to our active T3 hormone (which impacts gut motility)
It’s always important to consider both medications and supplementations and their potential side effects!
Getting Support with your SIBO
I recognize that this is a lot.
If you have SIBO — you’re probably just looking to get rid of it ASAP 🥲
If you’d like support not only navigating the SIBO itself, but would also like to investigate and address your deeper root causes so you don’t end up back here, I’d love love love to help you.
Inside my 1:1 program the Gut Restore Method, we’ll take that deeper root-cause approach to your SIBO, to make sure we’re not only addressing the overgrowth now, but accounting for the WHY so long-term relief is available to you.
If you’d like to learn more about the 1:1 program, and book in a discovery call to chat about whether it might be the right fit for you, you can do so here.
SOURCES:
GHT Academy Tier 1 Training